The Crisis of Antibiotic Misuse
 Centers for Disease Control and Prevention -
"Antibiotic resistance has been called one of the world’s most
pressing public health problems. It can cause significant danger and
suffering for people who have common infections that once
were easily treatable with antibiotics.
Centers for Disease Control and Prevention -
"Antibiotic resistance has been called one of the world’s most
pressing public health problems. It can cause significant danger and
suffering for people who have common infections that once
were easily treatable with antibiotics.
When antibiotics fail to work, the consequences are longer-lasting illnesses; more doctor visits
or extended hospital stays; and the need for more expensive and toxic
medications. Some resistant infections can cause death.
Sick individuals aren’t the only people who can suffer the consequences.
Families and entire communities feel the impact
when disease-causing germs become resistant to antibiotics.
These superbugs antibiotic resistant bacteria
can quickly spread to family members, school mates and co-workers;
threatening the community with a new strain of infectious
disease that is more difficult to cure and more expensive to treat."
The smart use of antibiotics is the key to controlling the spread of resistance.
Curtis Donskey MD - "Unfortunately, far too many physicians are still
thinking of antibiotics as benign.
We're just now beginning to understand how our normal microflora does
such a good job of preventing our colonization by
disease-causing microbes. And from an ecological point of view, we're
just starting to understand the medical consequences of
disturbing that with antibiotics."
A study published in the Journal of the American Medical Association (JAMA)
reveals that any use of antibiotics potentially increases the risk of
breast cancer in women. The specific data for this study states that women who took only
1 to 25 antibiotics over a 17 year period had a 1.5 times higher risk of breast
cancer as compared to women who took no antibiotics.
Antibiotics Can Change the Gut Microbiome for Up to a Year
 Doctors and patients alike should be thoughtful about starting antibiotics—not only
because of the well-publicized resistant bacteria that are proliferating thanks to
overuse of those drugs, but also because, a new study illustrates, there could be
serious consequences for the individual.
Doctors and patients alike should be thoughtful about starting antibiotics—not only
because of the well-publicized resistant bacteria that are proliferating thanks to
overuse of those drugs, but also because, a new study illustrates, there could be
serious consequences for the individual.
Martin Blaser’s 2011 article published in Nature highlights the potentially
dangerous long-term consequences that arise from the rampant overuse of antibiotics.
He argues that changes in our microbiome may even be promoting the transmission of
deadly organisms, as one of the important roles of an intact microflora is to
resist colonization by pathogenic organisms. Blaser also points out that not only does the individual use of
antibiotics cause permanent changes in the gut flora, but that infants
born to women given antibiotics during pregnancy, or the 30% of children
delivered via cesarean section, may be starting life with a significantly altered
nd insufficient level of friendly gut flora. This is a serious concern because
lack of diversity in friendly gut bacteria has been shown to contribute to a large number of diseases and complications.

Deadly Side Effects of Antibiotics
 Antibiotics are known to have side-effects; 'allergic' reactions to
antibiotics such as penicillin have been documented in
medical literature for over forty years. The severity of these
side-effects may range from a simple rash to anaphylaxis,
a life-threatening reaction which includes
difficult or labored breathing,
which are also symptoms of an asthmatic attack. It is now time to reconsider
whether the side-effects of
antibiotics should any longer be described as 'allergies', implying that the
problem lies with the patient rather than with the drug. It
is time that we acknowledged that drugs producing an 'allergic response'
are toxic, and in fact producing side-effects which are
in many cases symptomatic of poisoning.
Antibiotics are known to have side-effects; 'allergic' reactions to
antibiotics such as penicillin have been documented in
medical literature for over forty years. The severity of these
side-effects may range from a simple rash to anaphylaxis,
a life-threatening reaction which includes
difficult or labored breathing,
which are also symptoms of an asthmatic attack. It is now time to reconsider
whether the side-effects of
antibiotics should any longer be described as 'allergies', implying that the
problem lies with the patient rather than with the drug. It
is time that we acknowledged that drugs producing an 'allergic response'
are toxic, and in fact producing side-effects which are
in many cases symptomatic of poisoning.
The most common side effects with antibiotic drugs are diarrhea,
feeling sick and being sick. Fungal infections of the mouth,
digestive tract and vagina can also occur with antibiotics because they
destroy the protective 'good' bacteria in the body
(which help prevent overgrowth of any one organism), as well as the 'bad' ones, responsible for the infection being treated.
Rare, but more serious side effects, include the formation of kidney stones with the sulphonamides, abnormal blood
clotting with some of the cephalosporins, increased sensitivity to the sun with the tetracyclines, blood disorders with trimethoprim,
and deafness with erythromycin and the aminoglycosides. Sometimes, particularly in older people, antibiotic treatment can cause a
type of colitis (inflamed bowel) leading to severe diarrhoea.
Penicillins, cephalosporins and erythromycin can all cause this problem
but it is most common with clindamycin, an antibiotic usually reserved
for serious infections. If you develop diarrhea while taking
an antibiotic, immediately contact your doctor. Some people are allergic
to antibiotics, particularly penicillins, and can develop side
effects such as a rash, swelling of the face and tongue, and difficulty
breathing when they take them. Always tell your doctor or
pharmacist if you have had an allergic reaction to an antibiotic; sometimes the
reaction can be serious or even fatal. This is called an anaphylactic reaction.
Stuart Levy MD, Tufts University -
"People should realize that although antibiotics are needed
to control bacterial infections, they can have broad,
undesirable effects on microbial ecology. That is, they can produce long-lasting
change in the kinds and proportions of bacteria—and the
mix of antibiotic-resistant and antibiotic-susceptible types—
not only in the treated individual but also in the environment and society at large."
Revenge Of The Microbes: How Bacterial Resistance Is Undermining The Antibiotic Miracle
 Professor Graham Bell, from McGill University in Canada warns
that the new antibiotics pose" a serious and unprecedented" risk to public health. He warns that regulatory
authorities tend not to look many years ahead
when deciding whether to grant licenses to new drugs. "They are poorly designed
to detect even grave and highly probable
risks to public health arising from the population biology of microbes.
"Instead of dismissing the possibility that
widespread resistance will evolve, we should use the bitter experience that we have gained
from conventional antibiotics to plan for it."
Professor Graham Bell, from McGill University in Canada warns
that the new antibiotics pose" a serious and unprecedented" risk to public health. He warns that regulatory
authorities tend not to look many years ahead
when deciding whether to grant licenses to new drugs. "They are poorly designed
to detect even grave and highly probable
risks to public health arising from the population biology of microbes.
"Instead of dismissing the possibility that
widespread resistance will evolve, we should use the bitter experience that we have gained
from conventional antibiotics to plan for it."
Sarah Boseley- "The era of antibiotics is coming to a close.
In just a couple of generations, what once appeared to be
miracle medicines have been beaten into ineffectiveness by the bacteria they were designed to knock out.”
 Antibiotics are common cause of Candida. Antibiotics destroy both
harmful bacteria and good bacteria. When antibiotics destroy friendly bacteria it gives the Candida a chance to begin to multiply.
Anyone who has been treated with antibiotics for acne, major dental work or any condition where antibiotic use has been frequent,
more than 1 course of 7-10 days, is a prime candidate for Candida.
Antibiotics are common cause of Candida. Antibiotics destroy both
harmful bacteria and good bacteria. When antibiotics destroy friendly bacteria it gives the Candida a chance to begin to multiply.
Anyone who has been treated with antibiotics for acne, major dental work or any condition where antibiotic use has been frequent,
more than 1 course of 7-10 days, is a prime candidate for Candida.
Antibiotics are the acidic waste products of fermentation
Robert O. Young D.Sc., Ph.D. -
"Antibiotics are the acidic waste products of fermentation.
To make an antibiotic, you need a yeast or mold and some sugar for
the yeast or mold to ferment. The bi-product of the yeast or
mold fermenting the sugar is the acidic antibiotic. The acids from antibiotics DO NOT KILL BACTERIA.
They only force the bacteria to change.
Into what does bacteria change? Into yeast and mold. That is
why when you take antibiotics you end up with a yeast infection!
That's the antibiotic causing the bacteria to change from one form to
another. I call this process of change "biological transformation"
and the reason why you should NEVER take antibiotics."

Overuse and Misuse of Antibiotics in Pediatrics
 "Excessive antibiotics in children almost certainly stops normal
maturation of a healthy immune system. Lack of healthy bacteria in the
intestines caused by antibiotics creates an environment in which pieces
of partially digested proteins are able to penetrate the barrier of the
intestinal lining. When these abnormal proteins enter the blood the body
properly reacts to them as foreign substances. The foreign proteins cause
an antigen antibody reaction producing symptoms and setting the stage for
a possible auto-immune illness to develop. food allergies can also appear
along with impaired absorption of nutrients which may lead to poor health."
James Howenstine, MD.
"Excessive antibiotics in children almost certainly stops normal
maturation of a healthy immune system. Lack of healthy bacteria in the
intestines caused by antibiotics creates an environment in which pieces
of partially digested proteins are able to penetrate the barrier of the
intestinal lining. When these abnormal proteins enter the blood the body
properly reacts to them as foreign substances. The foreign proteins cause
an antigen antibody reaction producing symptoms and setting the stage for
a possible auto-immune illness to develop. food allergies can also appear
along with impaired absorption of nutrients which may lead to poor health."
James Howenstine, MD.
It is estimated that between approximately 70 to 80
percent of physician visits for sinus infections resulted
in a prescription for antibiotics. The problem lies in the
fact that these medications are designed only to attack
bacteria, not viruses. Yet, it is viruses which cause
the overwhelming majority of sinus infections (often
referred to as a "cold" or "the flu").
So, what is the harm? The answer is a phenomenon known as bacterial resistance to antibiotics.
Bacteria Antibiotic resistance is a widespread problem, and one that
in the U.S. Centers for Disease Control and Prevention
calls "one of the world's most pressing public health problems. In
a study published in The Lancet Infectious Diseases,
Dr. Tim Walsh at Cardiff University's team investigated cases of multi-drug
resistant Enterobactericeae infections - which include E.Coli and Salmonella.
 The spread of a drug-resistant bacterial gene could herald the end of antibiotics,
researchers warned us. Learn how to minimize your exposure to debilitating and often
life-threatening microbes by taking practical,
preventive measures to strengthen the immune system and accelerate immune response.
The spread of a drug-resistant bacterial gene could herald the end of antibiotics,
researchers warned us. Learn how to minimize your exposure to debilitating and often
life-threatening microbes by taking practical,
preventive measures to strengthen the immune system and accelerate immune response.
Stop Your Child's Ear Infections Naturally Without Antibiotics
 Antibiotics and ear tubes treat symptoms of a problem. Two out of three
infants receive antibiotics before they turn one year old. By the age of two,
three out of four children have received the drugs, according to recent research.
These findings are especially concerning as resistance to common antibiotics
is becoming an ever increasing problem. Deaths caused by Staphylococcus aureus,
the so-called superbug that is resistant to most antibiotics, are reportedly
increasing.
Antibiotics and ear tubes treat symptoms of a problem. Two out of three
infants receive antibiotics before they turn one year old. By the age of two,
three out of four children have received the drugs, according to recent research.
These findings are especially concerning as resistance to common antibiotics
is becoming an ever increasing problem. Deaths caused by Staphylococcus aureus,
the so-called superbug that is resistant to most antibiotics, are reportedly
increasing.
Moreover, research from a new study has shown that children from
low-economic backgrounds are more likely to receive antibiotics than those
from more well off families, and boys tend to receive antibiotics earlier
than girls. Low-economic background might be a factor because people from
this group tend to have higher rates of respiratory illness due to smoking and a lower likelihood of
breast-feeding.
They do not strengthen the organism so that it can fight the
infection itself, nor do they make the organism less resistant to
future infection. In chronic ear infection, it has become standard
procedure for physicians to use ear tubes in conjunction with
antibiotics or in place of it. These tubes help drain the pus
from the ear, but this treatment only deals with the results of
the problem; it does nothing to Alternatives to Antibiotics treat
the reason the infection was able to spread in the first place.
This physiological fact may be the reason ear tubes have been found to be of questionable value."

Antibiotic properties of glutathione
Skin and soft tissue infections (SSTIs) are growing in prevalence in both the outpatient
and inpatient settings and are some of the most common diseases seen by dermatologists,
who are often the first point of care for these patients. Microbial resistance to antibiotics
continues to rise as more virulent strains evolve, and strains predominantly found in the hospital
setting are now being seen in the community. Therefore, innovative approaches to combat this trend
are needed.
 Glutathione (GSH) is a well-described and established antioxidant. It participates in detoxification of xenobiotics,
regulation of cellular growth, modulation of immune response, and
maintenance of the thiol status of proteins and cellular cysteine levels. GSH is also known to have
a regulatory effect on immune cells and even inherent antibacterial properties have been reported.
To this end, the value of GSH as an antibiotic was evaluated by growing methicillin resistant
S. aureus, E. coli, K. pneumoniae and P. aeruginosa strains isolated from human skin and soft
tissue infection in the presence of GSH.
Glutathione (GSH) is a well-described and established antioxidant. It participates in detoxification of xenobiotics,
regulation of cellular growth, modulation of immune response, and
maintenance of the thiol status of proteins and cellular cysteine levels. GSH is also known to have
a regulatory effect on immune cells and even inherent antibacterial properties have been reported.
To this end, the value of GSH as an antibiotic was evaluated by growing methicillin resistant
S. aureus, E. coli, K. pneumoniae and P. aeruginosa strains isolated from human skin and soft
tissue infection in the presence of GSH.
At a physiologic concentration of 10 mM, GSH had no
effect on bacterial growth. At concentrations above 50 mM, which created acidic conditions (pH < 4),
bacterial growth was completely inhibited. When adjusted to physiologic pH, GSH exhibited a
bacteriostatic effect in a concentration-dependent manner. Additionally, the cytotoxicity
of GSH was evaluated in a murine cell line. GSH was relatively non-toxic to murine macrophages,
even at the highest concentration tested (160 mM). These results suggest the potential utility
of GSH for the prevention and/or as adjunctive treatment of infection, most significantly
in disease states associated with GSH deficiency.
Antibiotics and Yeast Infection -The Yeast Cell Overgrowth
More and more people are using antibiotics to cure minor infections, but have little clue that these types of medication are
playing havoc with their immune systems. Taking even the shortest course of antibiotic or steroid based medication can have a
catastrophic effect on your immune system,
kill the essential bacteria in your gut, and leave you wide open to other more serious infections.
 Antibiotics will kill off both the good and bad bacteria in your system,
and most of the essential bacteria in your gut will be killed or damaged. This good bacteria is what helps to keep the
yeast cells from overgrowing, but once they've gone, the yeast are free to grow and spread. Because the antibiotics have weakened
your immune system, your body will be helpless, and the yeast cells will be free to overgrow
further and spread to other areas of the body.
Once you've completed your course of antibiotics, it'll take your body weeks, and sometimes even months to re-build your immune system.
And, if a yeast infection takes hold, you could end up in serious trouble. A yeast
overgrowth will further weaken your immune system, and
before you know it, you'll end up catching every bug that's going around, you'll feel tired and run down all the time, and your yeast
infection will gradually get worse and worse.
Antibiotics will kill off both the good and bad bacteria in your system,
and most of the essential bacteria in your gut will be killed or damaged. This good bacteria is what helps to keep the
yeast cells from overgrowing, but once they've gone, the yeast are free to grow and spread. Because the antibiotics have weakened
your immune system, your body will be helpless, and the yeast cells will be free to overgrow
further and spread to other areas of the body.
Once you've completed your course of antibiotics, it'll take your body weeks, and sometimes even months to re-build your immune system.
And, if a yeast infection takes hold, you could end up in serious trouble. A yeast
overgrowth will further weaken your immune system, and
before you know it, you'll end up catching every bug that's going around, you'll feel tired and run down all the time, and your yeast
infection will gradually get worse and worse.
Dr. Lisa Landymore-Lin wrote all about this in her book Poisonous Prescriptions asking,
‘Do Antibiotics Cause Asthma and Diabetes?’ We are now even beginning to question the role of antibiotics as a cause of
cancer since they do lead to pathogen overgrowth especially in the area of yeast and fungi. Chris Woollams writes,
“It is estimated that 70 per cent of the British population have a yeast infection.
The primary cause of this is our love of antibiotics.

Antibiotics Put 142,000 Into Emergency Rooms Each Year.
U.S. Centers for Disease Control Waits 60 Years to Study the Problem
The US Centers for Disease Control (CDC) has just released
"the first report ever done on adverse reactions to antibiotics in the United States" on 13 Aug, 2008. (1)
This is "the first report ever"? How is that possible? Antibiotics have been widely used since the 1940s.
It is astounding that it has taken CDC so long to seriously study the side effects of these drugs. It is now apparent
that there have been decades of an undeserved presumption of safety.
Antibiotics can put you in the emergency room. Common antibiotics, the ones most frequently prescribed and
regarded as safest, cause for nearly half of emergencies due to antibiotics. And, incredibly enough, people in the
prime of life - not babies - are especially at risk. The study authors reported that "Persons aged 15-44 years accounted
for an estimated 41.2 percent of emergency department visits. Infants accounted for only an estimated 6.3 percent of ED visits."
They also found that nearly 80% of antibiotic-caused "adverse events" were allergic reactions. Overdoses and mistakes,
by patients and by physicians, make up the rest.
Allergic reactions to antibiotics may be very serious, including life-threatening anaphylactic shock.
Searching the US National Library of Medicine's "Medline" database (2) for "antibiotic allergic reaction"
will bring up over 9,700 mentions in scientific papers. A search for "antibiotic anaphylactic shock" brings up over 1,100.
Many papers on this severe danger were actually published before 1960. Given this amount of accumulated information,
one might wonder why CDC took so long to seriously study the problem.
 Overuse of antibiotics leads to antibiotic resistance. At its website, CDC currently states that antibiotic resistance
"can cause significant danger and suffering for people who have common infections that once were easily treatable with
antibiotics. . . Some resistant infections can cause death."
Overuse of antibiotics leads to antibiotic resistance. At its website, CDC currently states that antibiotic resistance
"can cause significant danger and suffering for people who have common infections that once were easily treatable with
antibiotics. . . Some resistant infections can cause death."
In the USA alone, "over 3 million pounds of antibiotics are used
every year on humans . . . enough to give every man, woman and child 10 teaspoons of pure antibiotics per year,"
write Null, Dean, Feldman, and Rasio. (5) "Almost half of patients with upper respiratory tract infections in the U.S.
still receive antibiotics from their doctor" even though "the CDC warns that 90% of upper respiratory infections,
including children's ear infections,
are viral, and antibiotics don't treat viral infection. More than 40% of about 50 million
prescriptions for antibiotics each year in physicians' offices were inappropriate."
Dr. Lawrence Wilson - "To strengthen the immune system,
one must address the needs of the whole body. A strong immune system is essential for health. It is a very complex system of the
body, involving the skin, intestines, nasal mucosa, blood, lymph and many other organs and tissues. Factors that impair the immune
system include nutrient deficiencies, contaminated air, water and food, unhealthful lifestyles and too much exposure to harmful
microbes. Other factors that weaken the immune system are negative attitudes and emotions and the presence of toxic metals,
toxic chemicals and biological toxins in the body. Others are sluggish metabolism, lack of rest and sleep, excessive stress
or too much exercise. As these causative factors are removed or corrected, the immune system improves."

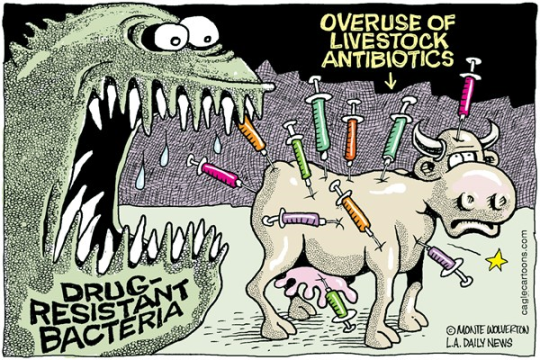
Antibiotics in Animal Feed is a Growing Public Health Hazard
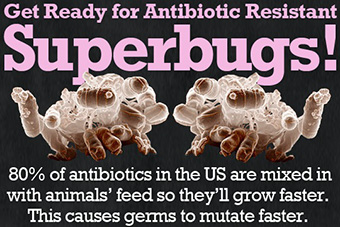 Currently, an estimated 70 percent of antibiotics and related drugs
in the United States are used in the feed and water of healthy animals
-- a practice with serious consequences for human health. Bacteria that are constantly
exposed to antibiotics develop resistance to these drugs.
When humans get sick from resistant bacteria, the antibiotics prescribed are less likely to work.
Currently, an estimated 70 percent of antibiotics and related drugs
in the United States are used in the feed and water of healthy animals
-- a practice with serious consequences for human health. Bacteria that are constantly
exposed to antibiotics develop resistance to these drugs.
When humans get sick from resistant bacteria, the antibiotics prescribed are less likely to work.
Experts have long known that the overuse of antibiotics by doctors and their patients has reduced the
ability of those drugs to cure infections. Now there is mounting evidence that the antibiotics widely used on farm
animals are also diminishing the power of important antibiotics to help people. Giving animals
antibiotics in their feed
can cause microbes in the livestock to become resistant to the drugs. People can then become infected with the resistant
bacteria by eating or handling meat contaminated with the pathogens. Resistant bacteria are
called Superbugs that cause pneumonia, urinary tract infections and skin infections are just a few of the dangers we now face.
"Many of us believe there is a tremendous overuse of antibiotics for animals," said Marcus Zervos, an infectious
disease specialist at William Beaumont Hospital in Royal Oak, Mich., who was involved in the Michigan case.
"There is some very strong opposition to our view that animal antibiotics are undermining antibiotics for people,
but this whole area has to be reconsidered." Most of the antibiotics used on the farm are not administered to treat sick animals.
Antibiotics Kill Your Body's Good Bacteria, Too, Leading to Serious Health Risks
"It is ironic that this humbled fungus, hailed as a benefactor of mankind, may by
its very success prove to be a deciding factor in the decline of the present civilization." -Dr. John I.
Pitt, The Genus Penicillum, Academic Press, 1979
Yeasts are opportunistic organisms. This means that, as the intestinal bacteria die, yeasts thrive, especially when their
dietary needs are met. They can use their tendrils, or hyphae, to literally poke holes through the lining of your intestinal wall.
This results in a syndrome called leaky gut. Yeasts are not the only possible cause of this syndrome. Some scientists have linked
non-steroidal, anti-inflammatory drugs (NSAIDS) such as naproxen and ibuprofen to the problem.
Given their ability to alter intestinal terrain, antibiotics
 also likely contribute to Leaky Gut Syndrome. In addition to possibly causing leaky gut syndrome,
I believe that parasitic yeasts can also cause you to change what you eat in that they encourage you to binge on carbohydrates
including pasta, bread, refined sugar, potatoes, etc. So, it should come as
no surprise that weight gain counts as one of the telltale signs of
antibiotic damage and subsequent yeast overgrowth.
also likely contribute to Leaky Gut Syndrome. In addition to possibly causing leaky gut syndrome,
I believe that parasitic yeasts can also cause you to change what you eat in that they encourage you to binge on carbohydrates
including pasta, bread, refined sugar, potatoes, etc. So, it should come as
no surprise that weight gain counts as one of the telltale signs of
antibiotic damage and subsequent yeast overgrowth.
By altering the normal terrain of the intestines, antibiotics can also make food allergies more likely.
An array of intestinal disorders can ensue, as well. Sadly, most doctors claim ignorance concerning their patient's intestinal
disorders rather than admit that the drugs they themselves prescribed actually caused the disorders to begin with.
Tons of antibiotics are fed to American livestock on a daily basis, purportedly to proof them against bacteria.
This practice not only possibly contributes to antibiotic resistance in humans -- many experts feel weight gain, and not disease
prevention, is the real reason antibiotics are so widely used. Fat cattle sell for more than thin cattle. That’s all very well, but
imagine what the antibiotics thereby possibly present in dairy products could be doing to our children’s health.
Probiotics are the beneficial bacteria that are normally present in the digestive tract. These bacteria are required for
proper digestion, the synthesis of Vitamin K, and the prevention of yeast infections and pathogen growth. Studies have shown
that the continual use of antibiotics has a devastating affect on the immune system. Each time you use an antibiotic,
the immune system gets further and further suppressed. Antibiotic kill friendly helpful microflora bacteria in a body,
not just the pathogenic bacteria. A healthy intestinal tract with a balanced microflora can boost the immune system,
keep pathogenic diseases of the intestinal tract in check. Probiotic use creates an intestinal environment that can
improve a user's immune system. The intestines are the body's largest immune organ. It's a fairly hostile environment
and a well balanced system can relieve immunological stress associated with an unhealthful system. This gives the immune system a chance
to enhance its capabilities in other parts of the body.

Are Antibiotics Making Your Animals Sick?
 Richard J. Holliday, DVM - "Antibiotics disrupt the normal population of beneficial
microbes in the gastrointestinal tract of all animals, these beneficial bacteria are the first fine of defense against most diseases,
without them the animal is more susceptible to other infections. Antibiotics depress the immune system by decreasing the
number of circulating white blood cells. This lowers the
animal's ability to fight infections. Some antibiotics, such as
chloramphenicol, can cause irreversible damage to the bone marrow. Many bacteria develop resistance to the effects of antibiotics,
This resistance can be passed to other bacteria, The concern is that if humans are exposed to resistant bacteria from animals
then the use of antibiotics may be Ineffective in treating any resulting
disease. This is the major controversy regarding the use of antibiotics on a regular basis in food producing animals."
Richard J. Holliday, DVM - "Antibiotics disrupt the normal population of beneficial
microbes in the gastrointestinal tract of all animals, these beneficial bacteria are the first fine of defense against most diseases,
without them the animal is more susceptible to other infections. Antibiotics depress the immune system by decreasing the
number of circulating white blood cells. This lowers the
animal's ability to fight infections. Some antibiotics, such as
chloramphenicol, can cause irreversible damage to the bone marrow. Many bacteria develop resistance to the effects of antibiotics,
This resistance can be passed to other bacteria, The concern is that if humans are exposed to resistant bacteria from animals
then the use of antibiotics may be Ineffective in treating any resulting
disease. This is the major controversy regarding the use of antibiotics on a regular basis in food producing animals."
Dr. Karen Becker DVM - "It’s vital to
understand that antibiotics do not discriminate
in the type of bacteria they destroy. They kill both the healthy and unhealthy bacteria. And, by decimating the good bacteria,
you increase your pet’s risk of subsequent intestinal infection and yeast overgrowth. Every time your pet is placed on
antibiotics. I strongly recommend you use a high quality
Probiotics, which replenishes the beneficial bacteria
the antibiotic destroys. I also recommend you ask your vet to perform
a culture and sensitivity test prior to guessing at which antibiotic will be effective for
treating your pet’s infection, unless the infection is life threatening.
Diarrhea, abdominal pain, severe inflammation of the colon (colitis), irritable bowel syndrome, skin problems,
fever, elevated white blood cell count, weak immune system, vomiting, dehydration, potassium deficiencies, allergies,
colon perforation, bad breath, excess stomach gas, yeast problems, nutritional deficiencies and constipation are just
some of the many side effects and problems linked to antibiotics. In 1928, when Alexander Glemming discovered
antibiotics, everyone was raving at this incredible breakthrough in medicine. However, over the years,
this breakthrough which was heralded with curing disease is now creating disease and problems of its own.
Bacteria now has built resistance to many antibiotics. Hence, stronger and stronger antibiotics are needed
to do the job and if weaker antibiotics create problems, can you imagine what more powerful antibiotics will do?
It's a vicious circle because ultimately bacteria will build resistance to the new and more powerful antibiotics too!
New forms of bacteria and disease are being created.
One of the reasons animals are becoming microbial resistant
too many of the antibiotics on the market is because vets take the
“here, try this one” approach to prescribing, which is the recipe for creation
of a dangerous superbug."These new problems are very dangerous and the flesh eating disease
is the best example of antibiotic resistant bacteria. Antibiotics literally means against life
(anti = against and biotic = life). In a healthy body, there is both good and bad bacteria in the intestinal tract.
There should be about 80% good bacteria and about 20% bad bacteria.
When antibiotics are used, both good and bad bacteria are destroyed in the intestinal tract.
Once the antibiotics are stopped, the bad bacteria grows back first and faster. The result is a very unhealthy and
weak body with no friendly bacteria. It takes on average 1 year to recover from antibiotics if you are feeding good
food and supplementing with friendly bacteria. If the diet you are feeding is bad, then your pet will take even longer to
recover and may never fully recover. Antibiotics relieve symptomatic problems but after the antibiotics are stopped,
the symptoms come back. So what happens now? They give more antibiotics. What's ironic is that antibiotics are then
given to help combat the problems that the antibiotics created in the body. Antibiotics are definitely over prescribed
and over used. Antibiotics for example do nothing for a virus and yet are often administered anyway.
Hopefully soon, common sense will prevail and medical practitioners will realize what is happening.
But, it is up to you, the people to put pressures on vets to become more careful about their practice of
administering antibiotics. In fact, encourage your vets to learn the alternatives. Make them aware that there are side effects
that can no longer ignored. Before antibiotics, what did people do? In World War 1, medics put
garlic cloves, long acclaimed for their natural antibiotic properties,
in the wounds of soldiers. Some use bee propolis which has natural phagocystosis properties. Phagocystosis is
the ability to encourage white blood cells to
destroy bacteria. There are certainly many other natural antibiotics which have no side effects
(except bad breath in garlic's case). In general, natural antibiotics only attack bad bacteria and leave
the friendly bacteria alone. Become aware that although antibiotics have helped save many lives,
they are not a cure by any means.
Conclusion
- The body should have 80% friendly bacteria and about 20% bad bacteria inside the intestinal tract. After the use
of antibiotics, the body will have no more than 20% friendly bacteria and 80% bad bacteria if not more.
-Most illness, disease and problems begin in the intestinal tract. Thus, antibiotics
create the potential for serious illness to begin.
-You may not be giving your pet antibiotics, but if it has ever eaten foods with preservatives, you have been giving
your pet what I call 'hidden antibiotics'. The job of preservatives is to control bacteria and once your pet eats food with
preservatives, it will ultimately have an effect inside the intestinal tract too and kill the friendly bacteria.
-You should expect it will take at the very least 1 year to recolonize the intestinal tract with
friendly bacteria after the use of antibiotics.
-Recolonize the intestinal tract with friendly bacteria by using supplements and feeding natural foods.

Antibiotics and Suppressive Therapies
Although the suppressive therapies are hard on the body, they do not compare with he rampant idiocy of
using antibiotics for viral infections. Thankfully some measure of sanity appears to be returning to the medical profession.
More and more doctors are avoiding prescribing antibiotics for colds and flus. Several critical observations must be made here.
First, antibiotics are totally ineffective against viruses. The excuse most often heard for prescribing antibiotics
in a viral illness is to prophylactically protect the body against a secondary bacterial infection. This is an idea proven to be
false decades ago. In the United States, of the 5 most common antibiotics prescribed, three are broad spectrum. That's a problem!
Second, the basis of antibiotics is mold. Through millions of years of evolution, bacteria and mold have
coexisted in nature - in the soil, plants and animals. When one of them developed an evolutionary edge over the other
and began to shift the balance in favor of itself, the other must have rapidly learned to defend itself against this new attack.
If this were not true, we would only have either bacteria or molds but not both. By using mold, we thought we could slay
one step ahead of bacteria in the evolutionary scale because we're so smart. Well, the yolk is on us, the bacteria are winning,
and at a record pace. So in our attempt to wipe out bacteria, we forced them into a revolutionary evolutionary change
and we damaged our immunity so badly that we become easy prey for viruses. Additional side effects of antibiotics are
immune suppression and the increased susceptibility to parasites.
The long term effects of the breakdown of the immune system can be seen in increased infections, auto-immune
disorders and tumor formation. The body's last ditch effort to compensate for the loss of internal defenses is to hyper activate
the depressed immune function. What it may do is over stimulate the immune function,
sacrificing the "self" - "not self" regulatory mechanisms. The defenses then perceive its own organs and systems
as "not self" and begin to mount defenses against them. This starts the precipitous march toward auto
immune disorders such as SLE, MS, RA, and possibly CFS.
New strains of vancomycin-resistant enterococci (VRE)
In 1988 in a New York City hospital, the first strains of vancomycin-resistant enterococci (VRE) appeared, and
between September 1989 and October 1991, 38 New York hospitals reported VRE infections, 98 percent of which were
contracted during the patient's hospital stay. Soon hospitals in New Jersey, Connecticut and other states began reporting
VRE infections, and the problem quickly spread to other countries. VRE infections are now a worldwide problem.
Nearly all VRE infections are acquired in hospitals. The longer the hospital stay, the greater the risk.
Although the risk is highest in intensive care units, VRE infections in hospitals have been traced to nearly every
patient-occupied area. Individuals previously treated with vancomycin or combination antibiotic therapy have an
increased risk of developing VRE. Those with a serious disease or suppressed immune system or who undergo abdominal
surgery are at increased risk. Most VRE infections occur in patients 41 to 60 years old, but they can affect people of any age.
VRE infections are virtually not treatable using conventional methods. Even if combination antibiotics appear to be effective,
the patient soon has a relapse more virulent than the original infection. A 1995 study at Albert Einstein College of Medicine in
New York found that when VRE infections spread to the blood (bacteriemia), the in-hospital death rate was 100 percent.
VRE infections are now the second leading cause of infections acquired in hospitals.
Warming oceans are the new breeding grounds for pathogens
Hospitals are not the only breeding ground for new versions of old pathogens. As the New York Times explained on
January 24, 1999, previously unknown bacteria and viruses are blooming in the earth's warming oceans, killing marine
life and threatening human health. At that week's national meeting of the American Association for the Advancement of Science,
researchers reported that dying coral, diseased shellfish
 and ocean waters infected with human viruses are symptoms of a rapidly growing global problem.
and ocean waters infected with human viruses are symptoms of a rapidly growing global problem.
According to the organization, new studies show that vast colonies of human viruses migrate regularly into
Florida's coastal waters from the state's 1.6 million septic tanks, and many people are becoming infected with viruses
picked up while swimming, windsurfing or boating in infected waters. One study found that almost 25 percent of the
people using marine beaches developed ear infections, sore throats, sore eyes, respiratory infections or gastrointestinal
disease. Some of the viruses detected in coastal waters are linked to heart disease, diabetes, meningitis and hepatitis.
“Most people who come in contact with these viruses do not get ill,” said Joan B. Rose,
a researcher at the University of South Florida, “but of the 20 to 24 percent who do, about
1 percent become chronically infected.” Rose's research team traced the migration of
viruses from septic tanks and found that pathogens infect coastal waters within 24 hours
of being flushed down toilets. Storms that churn ocean water speed the process. Many of
the viruses that infect humans directly or through the eating of contaminated shellfish
cannot be detected by the routine monitoring of water pollution. Other researchers at the
meeting said that the increase in pathogens in the world's oceans may be linked to a
1.8-degree rise in ocean surface temperatures detected in many area
Vol. 9, No. 1 ~ January/February 2000
"It is ironic that this humbled fungus, hailed as a benefactor of mankind, may by its very success prove to be a
deciding factor in the decline of the present civilization." - Dr. John I. Pitt, The Genus Penicillum, Academic Press, 1979